Should scientists become gene genies?
ASU Professor James Collins, part of government advisory panels on CRISPR technology, weighs in on latest experiment

Scientists have for the first time edited genes in human embryos to fix a disease-causing mutation, according to a paper published (ironically) in the journal Nature.
They used a new, cheap and radical tool that enables geneticists and researchers to edit genomes easily by removing, adding or altering sections of DNA.
The technology is known as CRISPRCRISPR stands for Clustered Regularly Interspaced Short Palindromic Repeats., and the fears — and there are many — are that it could be used for human enhancement. Think super soldiers, or parents who create super kids to ensure success in life. Or that it could be used to create designer organisms that wreak havoc in nature. Or that it could be used to wipe out all mosquitos, when science does not yet know what function mosquitos perform in the wider ecosystem.
Two government advisory panels came out with dueling recommendations in the past 12 months. James Collins, Virginia M. Ullman Professor of Natural History and the Environment in the School of Life SciencesThe School of Life Sciences is in the College of Liberal Arts and Sciences. at Arizona State University, sat on one of them.
Collins was co-chair of the National Academy of Sciences' Committee on Gene Drive Research in Non-human Organisms: Recommendations for Responsible Conduct, a panel of 16 experts who released a lengthy report called “Precaution and governance of emerging technologies” in June.
ASU Now sat down to discuss the development with Collins.
“It’s a fascinating step in the use of this new CRISPR technology in terms of gene editing, opening up the possibility of using it in a variety of circumstances, whether it’s non-human animals or human beings,” Collins said. “It’s a fascinating technology that’s raising a lot of questions.
“It was in December of 2016 that the National Academy of Sciences held a meeting of international experts to discuss the possibility of using CRISPR for editing human embryos. It was at that meeting that they adopted a motion that the technology should not be used for editing human embryos, at least at this time. At the same time that meeting was going on, there was a committee of the National Academy of Sciences working on just this issue: Should CRISPR and other gene-editing technologies be used for editing the human germline in particular?”
Question: Changes to the germline are hereditary, correct?
Answer: That’s correct. Changes to the germline would be hereditary. They would go from one generation to the next.
Q: The panel endorsed only alterations designed to prevent babies from acquiring genes known to cause “serious disease and disability” and only when there is no “reasonable alternative.”
A: Exactly. That committee, in their report, came out with that recommendation, which is actually contrary to the recommendation that came out in December 2016. So you had two different opinions on the table.
Q: So there’s no consensus on this?
A: No, certainly in the larger community there would be no consensus. The community would be divided in a number of different ways, with one extreme — “Don’t do any gene editing at all” — and the other would vary gene editing under conditions as were described in that quote — serious, possibly lethal, mutations — that could be corrected, and then it would be appropriate to think about using the gene-editing technology, and not using the editing if it was just a question of enhancement.
Then the question becomes what counts as enhancement and what doesn’t count as enhancement? How do you make that decision? So, no, there’s not a consensus at this point.
Q: Do you think the experiment cited in the Nature paper was a toe dip on a slippery slope?
A: What it is is one more step of modifying human beings. In this case it’s going to be modifying human embryos. As the National Academy of Sciences put it, they open up the door to doing this sort of work in just this sort of circumstances. It’s an ideal case in this regard, where you can just reach in and you have a mutation and major defect and the change can be made and the embryo will develop without the defect, if everything works OK. That’s just the case the National Academy was looking towards. So is it a slippery slope?
The question then becomes — as far as the National Academy is concerned — when are you in a condition such as this where there’s a straightforward need as far as the viability of the embryo is concerned as opposed to just enhancement. Then you’re back to the question of what constitutes enhancement, and who makes that decision. That’s not clear-cut. My recollection is that the National Academy report authors were not clear on that either.
Q: What if a child produced through gene editing were hobbled in some unforeseen way?
A: Presumably that is going to be the kind of possibility that would be taken under consideration before this sort of technology is approved ultimately for use in human beings in a clinical environment. This is an experimental environment at this point. ... It’s just in a laboratory.
The question that you pose — an untoward effect — is something that’s going to have to be taken into consideration by the group that ultimately would approve the first clinical trials with this sort of technology. That would be the sort of consideration that would come into play when any sort of clinical intervention is considered. There’s always a risk associated with it, and the question would be what counts as a tolerable risk?
Q: Clearly there’s a lot more discussion that needs to happen about this technology.
A: There’s a lot more discussion that’s going to have to happen on the side of the ethical, legal and social implications of this sort of work. There’s a lot more discussion that’s going to have to happen on the research side as well.
There’s still a good deal of research to take place in order to fine-tune this technology for the purposes of making this as precise as possible so that the risk is going to be minimized. Which is what you’d want to do with any technology.
More Science and technology
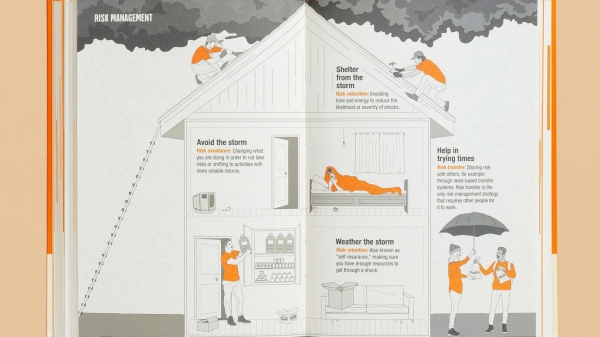
ASU author puts the fun in preparing for the apocalypse
The idea of an apocalypse was once only the stuff of science fiction — like in “Dawn of the Dead” or “I Am Legend.” However these days, amid escalating global conflicts and the prospect of a nuclear…

Meet student researchers solving real-world challenges
Developing sustainable solar energy solutions, deploying fungi to support soils affected by wildfire, making space education more accessible and using machine learning for semiconductor material…
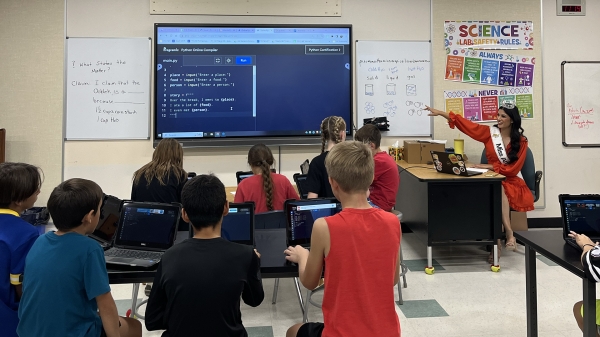
Miss Arizona, computer science major wants to inspire children to combine code and creativity
Editor’s note: This story is part of a series of profiles of notable spring 2024 graduates. “It’s bittersweet.” That’s how Tiffany Ticlo describes reaching this milestone. In May, she will graduate…